
:max_bytes(150000):strip_icc()/GettyImages-149957567-5710592d3df78c3fa27f3328.jpg)
Bivariate analyses indicated a high level of relationships among the HIV sexual risks and other factors. Face-to-face, computer-assisted, structured interviews were conducted with 1535 individuals in Atlanta, Georgia. The objective is to examine multiple factors associated with sexual HIV risk behaviors within a syndemic conceptual framework. The focus of this paper is on HIV sexual risk taking among a community-based sample of disadvantaged African American adults. Therefore, interventions intended to empower CCU among women need to expand beyond acknowledging the reduced control that women who use drugs demonstrate to also consider those who have drug-using sexual partners. Women with drug-using partners, especially a steady partner, were least likely to report CCU. Among non-drug users, having a drug-using partner was associated with decreased odds of condom use for women only. Having a steady partner decreased the odds of CCU, while higher condom use self-efficacy increased the odds of CCU. The sample included 1,357 African American men and women (M age 37.0, SD 13.1 years 44% women, 66% men) from 61 disadvantaged census block groups in Atlanta, GA as part of a study of individual and neighborhood characteristics and HIV risk-taking. This study focused on the effect of sex partner type (steady versus casual), drug use, and condom use self-efficacy regarding consistent condom use (CCU) among a community-based sample of adults. Gender inequalities in sexual behavior are explored from the perspective of the theory of gender and power. Findings indicate the continued need to consider sex in the context of drug use, and reveal the importance of measuring such influences and all antecedents of condom use separately for steady versus casual sexual relationships. Personalized norms regarding condom use were not salient factors in predicting increased rates of condom use with either partner type.
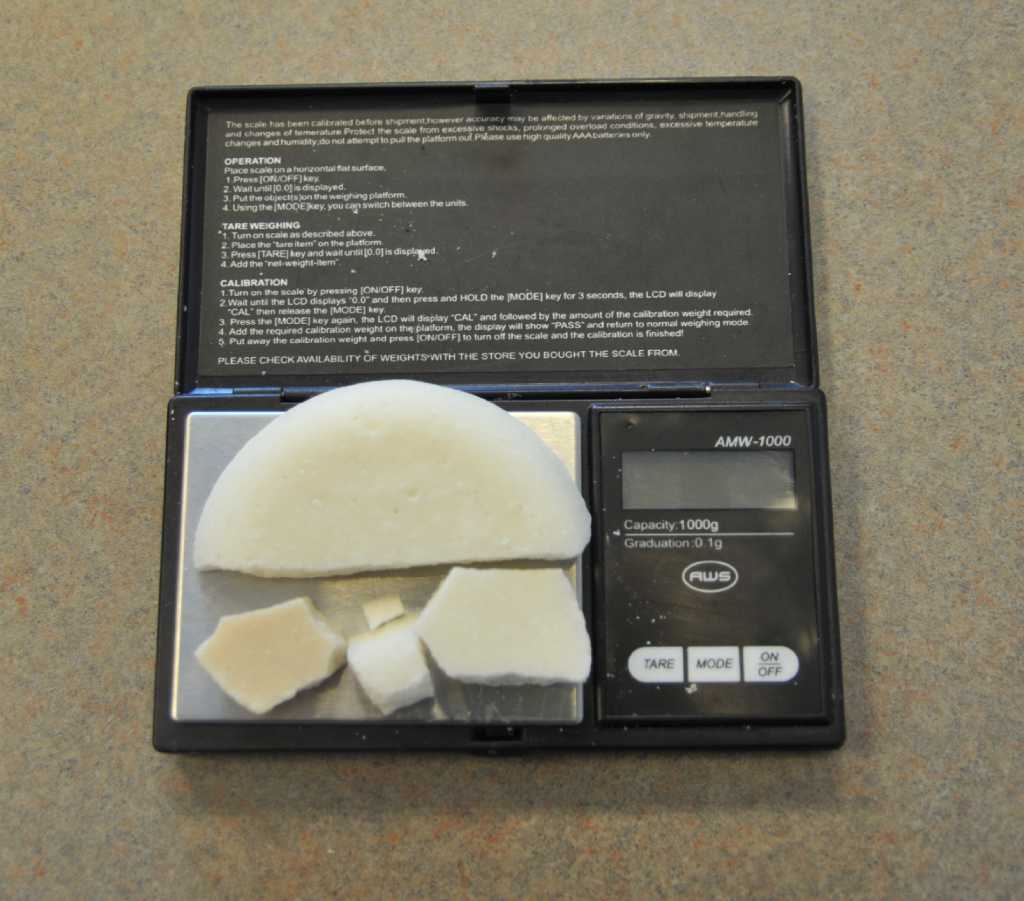
#MEDICINE BYWORD FOR CRACK CRACK#
Condom use with casual paying partners was associated with having sex while high and the frequency of crack cocaine use. Increased condom use with steady partners was associated with drug-using status, intervention assignment, sexual relationship characteristics, age at first condom use, and HIV testing history. Predictors of condom use with steady and casual paying partners were examined separately. Data were analyzed from 138 women (aged 18 to 59), recruited from inner-city Atlanta (Georgia, U.S.) neighborhoods. Predictors of increased male condom use are investigated following a recent, gender-specific HIV intervention among African-American women. The emergence of crack cocaine injection requires urgent attention, as this new drug use behavior is associated with elevated rates of high risk behaviors.

Crack injectors reported higher rates of abscesses, mental illness and Hepatitis C infection, but not Hepatitis B or HIV infection. After adjusting for current (past 30 day) speedball and powder cocaine injection, crack injectors reported higher rates of risky drug use behaviors and female crack injectors reported higher rates of risky sexual behaviors. Significant differences were found on race, education, employment and residence, with crack injectors more likely to be white, employed, better educated and living in New Haven than IDUs who have never injected crack. Lifetime and current crack injectors did not differ on gender, age or marital status from IDUs who have never injected crack. Lifetime and current crack injectors did not differ significantly on any demographic characteristics. Nine percent (n = 89) of participants reported "ever" injecting crack cocaine and 4.2% (n = 42) reported injecting crack in the past 30 days. Participants were administered a modified version of the National Institute on Drug Abuse Risk Behavior Assessment Questionnaire. Nine hundred and eighty-nine IDUs were recruited in New Haven, CT, Hartford, CT and Springfield, MA from January 2000 to May 2002. To compare demographic, HIV risk behaviors, and health status characteristics of injection drug users (IDUs) who have injected "crack" cocaine with IDUs who have not.


 0 kommentar(er)
0 kommentar(er)
